The Ultimate Guide to Nursing Diagnosis in 2024
The Ultimate Guide to Nursing Diagnosis in 2024
Nursing diagnosis is an essential part of the nursing process. It helps nurses identify and manage patient-specific problems through assessment, planning, implementation, and evaluation. In 2023, nurse practitioners will need to be prepared to use nursing diagnoses with greater accuracy and precision than ever before.
This ultimate guide to nursing diagnosis in 2023 provides comprehensive information on the latest developments in nursing diagnosis technology and research and offers practical guidance for both nursing students and practitioners on making the most of this vital tool.
Introduction
Welcome to the ultimate guide to nursing diagnosis in 2023! As a nurse practitioner, you know how important it is to accurately diagnose patients. With the advances in technology and research that have taken place in nursing knowledge in recent years, this guide will help you stay up-to-date on the latest developments in nursing diagnosis and provide practical guidance for using this important tool.
We’ll cover all of the essentials: What are the types of nursing diagnosis? How did it develop? What are some of the risks associated with this type of nursing diagnosis? What is the future of nursing diagnosis in 2023? Finally, we’ll provide tips and tricks for using this essential tool effectively.
Definition and Overview of Nursing Diagnosis
Nursing diagnosis is a process for clinical decision-making that helps nurses identify and manage patient-specific problems through assessment data analysis, planning, implementation, and evaluation.
It involves gathering data about the patient’s condition to arrive at an informed conclusion about their health status. This includes assessing patient symptoms, evaluating the patient’s health history, and current condition, and making an informed decision about how to intervene.
History and Development of Nursing Diagnosis
Nursing diagnosis has been around since the 1960s when Florence Nightingale first proposed a systematic approach to nursing care. Over the years, this approach has evolved into a more sophisticated system that includes assessment, diagnosis, intervention, and evaluation.
In recent years, technology has played an important role in advancing nursing diagnosis by allowing nurses to access greater amounts of data and quickly analyze it. This has enabled nurses to make more accurate diagnoses, which has led to better outcomes for patients.
Risk Nursing Diagnosis
While nursing diagnosis is an invaluable tool, it is not without risks. One of the most common risks associated with a nursing diagnosis is misdiagnosis, which can lead to incorrect or no diagnosis focusing on inadequate treatment plans nursing, and medical interventions.
Additionally, if a nurse does not properly assess the patient’s condition before making a diagnosis, they may miss vital symptoms that could affect the patient’s health status and actual or potential health prognosis.
What Is Risk Nursing Diagnosis?
Risk nursing diagnosis is an important part of the clinical decision-making process that nurses must be aware of when making a potential nursing diagnosis call. This type of nursing risk diagnosis often involves assessing and evaluating the patient’s risk for certain conditions or diseases based on their symptoms, medical history, lifestyle, and other factors. Risk nursing diagnoses help to identify patients who are at high risk for certain conditions and can inform treatment plans accordingly.
It is important to note that risk nursing diagnoses are not intended to replace traditional nursing diagnoses, but rather provide an additional layer of information.
Process of Nursing Diagnosis
The process of nursing diagnosis can be broken down into four key steps: assessment, diagnosis, intervention, and evaluation.
The first step—assessment—involves gathering patient data-related factors such as symptoms, medical history, lifestyle, and other relevant factors. This will help to identify any actual or potential health issues that need to be addressed.
Once the nurse has completed the assessment phase, they can then move on to making a diagnosis. During this step, nurses use their experience and knowledge to decide how best to intervene to manage the patient’s condition.
The third step of syndrome diagnosis is intervention, which involves advanced healthcare practitioners taking action to help the patient manage their condition. This could include prescribing medications, ordering tests, providing lifestyle advice, or arranging for further treatment.
Finally readiness for enhanced well, the fourth step is evaluation. During this phase, nurses assess the effectiveness of their interventions and make necessary adjustments to improve patient outcomes.
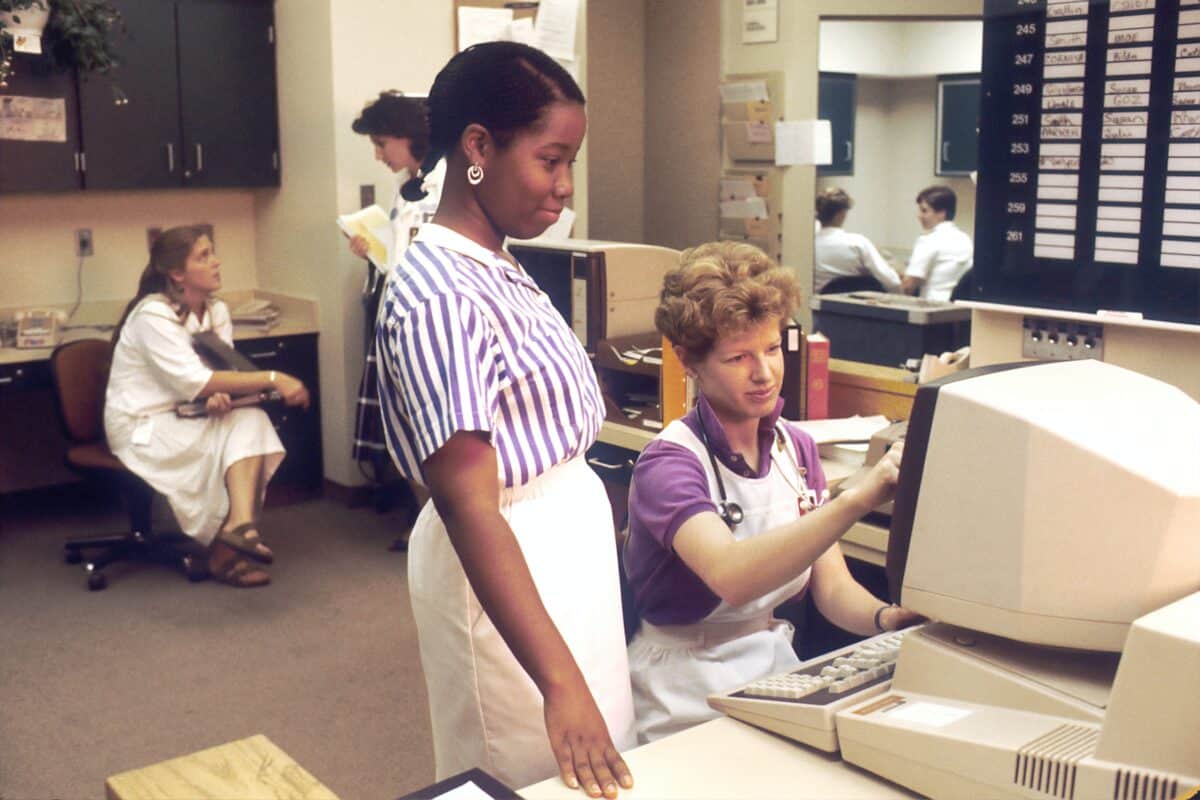
Technology Advancements in Nursing Diagnosis
In 2023, nurse practitioners can expect to see even more advances in nursing diagnosis technology. With the help of artificial intelligence (AI) and machine learning algorithms, nurses will be able to access and analyze larger amounts of data more quickly than ever before.
These technologies will also allow for the development of more sophisticated diagnostic tools that can provide improved accuracy and precision when making diagnoses.
In addition to AI and machine learning, recent advancements in telemedicine technology are making it easier for nurses to access remote patient monitoring, which can be used in conjunction with traditional nursing diagnosis methods.
Artificial Intelligence (AI) – How It Enhances Nursing Diagnosis?
Artificial intelligence (AI) is playing an increasingly important role in nursing diagnosis.
AI-based algorithms can quickly analyze vast amounts of data, allowing nurses to more accurately and efficiently diagnose patients. AI systems are also capable of deep learning which enables them to improve their accuracy over time by recognizing patterns in the data.
AI technologies can be used to develop diagnostic tools that can supplement traditional nursing assessment methods. These tools can provide nurses with improved accuracy when diagnosing conditions such as diabetes, hypertension, and other chronic illnesses.
Tips and Tricks for Successful Nursing Diagnosis
Although technology has made nursing diagnosis easier, it is still important to follow some key tips to ensure that diagnoses are accurate and timely.
Here are some tips for successful nursing diagnosis:
• Assess the patient’s condition thoroughly before making a diagnosis.
• Carefully consider the patient’s history before making any treatment decisions.
• Utilize available technological resources such as AI-based diagnostic tools to supplement traditional assessment methods.
• Ask questions to ensure you have a comprehensive understanding of the patient’s symptoms.
• Make sure to document all assessments and diagnoses in case they are needed for future reference.
Mobile Technology – Bringing Nursing Diagnosis to the Patient’s Bedside
Mobile technology is revolutionizing the way nurses diagnose patients. By bringing nursing diagnosis to the patient’s bedside, mobile technology enables nurses to more quickly and accurately diagnose a wide range of conditions.
For instance, mobile devices such as smartphones and tablets allow nurses to access remote patient monitoring systems so they can assess vital signs on-site. This eliminates the need for long wait times while lab tests are conducted or results are returned from specialists.
In addition, mobile technology allows nurses to access and analyze larger amounts of data quickly and accurately. This can be especially beneficial when diagnosing complex conditions such as cancer, heart disease, and stroke.

Nursing diagnosis is an essential part of providing quality healthcare. As technology continues to evolve, nurses should expect to see more advances in nursing diagnosis techniques in the coming years.
By utilizing AI-based algorithms, telemedicine technologies, and mobile devices, nurses can gain a better understanding of their patient’s conditions and provide more accurate and timely diagnoses.
With these advances, the ultimate guide to nursing diagnosis in 2023 should be a powerful tool for providing quality patient care.
Virtual Reality (VR) – Improving Access to Diagnostic Tools
Virtual Reality (VR) is another exciting technology that can be used to enhance the nursing diagnosis process.
VR can help nurses better assess and diagnose a patient’s condition by allowing them to interact with 3D medical models, enabling them to gain a more comprehensive understanding of the patient’s anatomy and physiology.
VR can also provide nurses with access to advanced diagnostic tools such as MRI, CT scans, and X-rays. By using these technologies, nurses can gain a much clearer picture of what is going on inside the patient’s body and make more informed decisions about the best way to treat their condition.
By utilizing all the latest technologies, nurses can gain a more comprehensive understanding of their patient’s conditions and provide better diagnoses in less time. AI-based algorithms, mobile devices, virtual reality, and telemedicine technologies are all powerful tools that can help nurses improve their ability to diagnose medical conditions accurately and efficiently.
Medical Diagnosis By Nurses
Nursing diagnosis is a critical part of providing quality healthcare, and nurses play an essential role in the process of clinical judgment.
Nurses are responsible for assessing a patient’s condition, gathering information from lab tests and other sources, and interpreting the data to make an accurate diagnosis. By using their expertise, nurses can help identify underlying conditions to ensure that patients receive the most effective treatment plan.
When making a nursing diagnosis, nurses need to utilize all available medical resources and evidence-based practice guidelines. This means considering both traditional methods and components of a nursing diagnosis, such as physical examination and lab tests, as well as more advanced technologies such as AI-based algorithms, telemedicine technologies, and virtual reality.
By taking into account all of the available evidence, nurses can make more informed decisions about their patient’s condition and provide better treatment plans that lead to improved outcomes.
Current Research in Nursing Diagnosis
Nursing diagnosis is an ever-evolving field, and current research in this area continues to uncover new insights into patient care.
With the help of AI-based algorithms, remote monitoring systems, and virtual reality technologies, nurses can gain a more thorough understanding of their patient’s conditions in much less time than ever before.
For instance, AI-based algorithms allow healthcare professionals to quickly analyze large amounts of data and uncover hidden patterns that they may have otherwise missed. This can be especially helpful when diagnosing rare or complex conditions.
Telemedicine technologies also enable nurses to provide care to patients who may not otherwise have access to medical services, such as those living in rural areas. By using remote monitoring systems, healthcare professionals can assess vital signs and diagnose conditions from a distance.
In addition, virtual reality technologies are being used to simulate medical procedures and allow healthcare professionals to practice their skills in a safe environment. This helps them build confidence in their abilities and understand the anatomy of their patients better.
By utilizing all the latest technologies, nurses can provide better diagnoses in less time. This will help improve patient care and ensure that everyone receives the necessary treatment they need.
Improved Decision-Making Through Predictive Analytics
Predictive analytics is a powerful tool that can help nurses make better decisions when it comes to diagnosis. By utilizing AI-based algorithms, healthcare professionals can quickly analyze data and uncover patterns that may have otherwise been missed.
This helps them make more informed decisions about a patient’s condition and helps them provide the best care possible.
For instance, predictive analytics can be used to identify and assess risk factors that may influence a patient’s diagnosis. By analyzing a range of variables such as age, gender, lifestyle choices, and past medical history, healthcare professionals can develop an accurate picture of a patient’s condition and make the best treatment decisions possible.
The actual nursing diagnosis process has come a long way in the past few years thanks to advances in technology. AI-based algorithms, remote monitoring systems, virtual reality technologies, and predictive analytics are all powerful tools that can help nurses diagnose conditions more accurately and efficiently. As technology continues to evolve, we can expect even more innovation in the field of nursing diagnosis in the future.
Evidence-Based Practice and Nursing Diagnosis
Evidence-based practice is becoming increasingly important in the field of nursing diagnosis.
By utilizing evidence-based practices, nurses can make sure their diagnoses are based on the most up-to-date medical research and treatments. This helps ensure that patients receive the most effective care possible.
To ensure that nursing diagnoses are based on the most current evidence, nurses should regularly read peer-reviewed journals and attend conferences to stay informed of new developments in the field. They should also be familiar with research methods such as randomized controlled trials, systematic reviews, and meta-analyses so that they can accurately assess the level of evidence for a given diagnosis.
In addition, nurses should develop a thorough understanding of medical coding systems and documentation standards so that they can properly record their diagnoses. By keeping accurate records, healthcare professionals can more easily track patient progress and ensure that everyone receives the necessary treatments.
By utilizing evidence-based practices and staying up to date with the latest developments in nursing diagnosis, healthcare professionals can provide better care to their patients and improve outcomes.
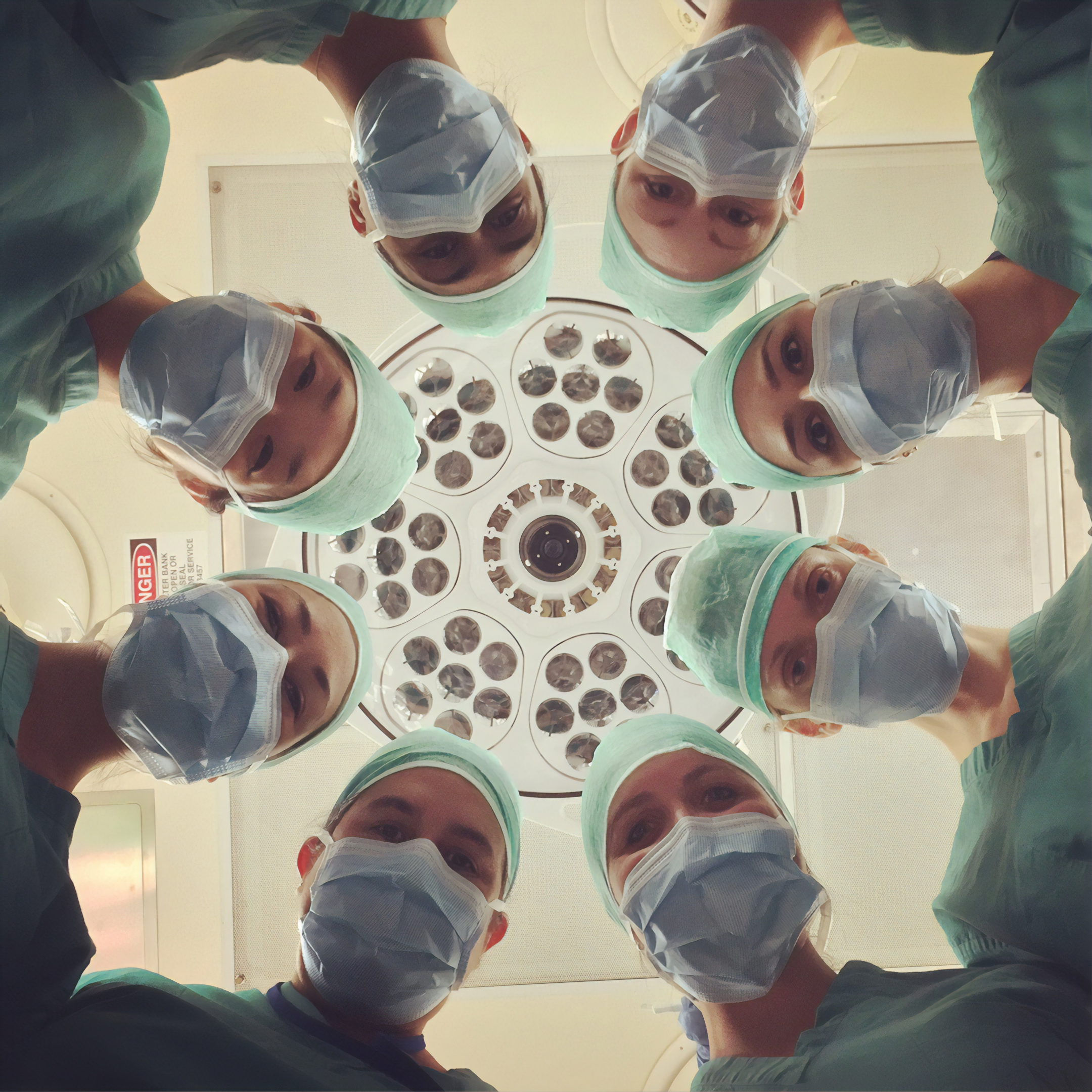
Interdisciplinary Collaboration for More Effective Nursing Diagnoses
Interdisciplinary collaboration is an essential part of effective, nursing interventions and diagnoses. Working together with other healthcare professionals, such as doctors, physical therapists, and pharmacists, can help nurses make more informed decisions about their patient’s conditions.
By collaborating, healthcare professionals can exchange ideas and develop a better understanding of the patient’s needs.
In addition to improved decision-making, interdisciplinary collaboration can lead to better patient outcomes. For instance, by working together to develop a plan of care that is tailored to the individual patient’s needs, healthcare professionals can ensure that the patient receives the most effective treatment possible.
To maximize the benefits of interdisciplinary collaboration, healthcare providers should create a culture of communication and trust among their teams.
Nurses should work to foster an atmosphere of open communication between team members to ensure that everyone is working together to provide the best care for their patients.
Practical Strategies for Improving Nursing Diagnosis in 2023
As healthcare technology continues to evolve and the demand for quality nursing diagnoses increases, nurses need to implement practical strategies to ensure that their diagnoses are accurate.
With the right strategies in place, nurses can provide better care for their patients and improve outcomes.
Developing a Skillset for Accurate Nursing Diagnoses
As healthcare technology advances, nurses must develop the skills necessary to make accurate diagnoses. This requires an understanding of the latest evidence-based practices, interdisciplinary collaboration techniques, and practical strategies.
To start, nurses should read peer-reviewed journals and attend conferences regularly to stay informed of new developments in the field. They should also be familiar with research methods such as randomized controlled trials, systematic reviews, and meta-analyses so that they can accurately assess the level of evidence for a given diagnosis.
Additionally, nurses should understand the various medical coding systems and documentation standards so that they can properly record their diagnoses. By keeping accurate records, other healthcare providers and professionals can more easily track patient progress and ensure that everyone receives the necessary treatments.
As nursing diagnoses become increasingly complex, nurses need to develop a skill set that allows them to make accurate diagnoses. By staying up to date with the latest developments in nursing diagnosis, utilizing evidence-based practices, and fostering an atmosphere of interdisciplinary collaboration, nurses can provide better care to their patients and improve outcomes.
Creating a Comprehensive and Evidence-Based Care Plan
Having an evidence-based care plan is essential for providing the best care possible to your patients. A comprehensive care plan should include a detailed assessment of the patient’s condition, as well as clear steps for treatment and follow-up.
One strategy that healthcare providers can use to create an effective care plan is to develop a checklist of all the elements that need to be included. This checklist should include patient information, such as medications, allergies, recent lab tests, and treatments, as well as a detailed plan of action.
In addition to the checklist, healthcare providers should also develop an evidence-based care plan that outlines the expected outcomes for each step of the treatment and follow-up process. This will help ensure that all treatment decisions are based on scientific evidence and best practices.
Finally, healthcare providers should make sure to document any changes in the patient’s condition or treatments so that they can track progress over time. Accurate documentation is essential for providing quality care and ensuring positive patient outcomes.
Utilizing Advanced Technology To Streamline Processes
As healthcare technology advances, nurses should take advantage of the latest tools to streamline processes and improve patient care. For instance, nurses can use electronic health records (EHRs) to document patient information quickly and accurately.
By integrating EHRs into their workflow, nurses can save time and reduce errors in record keeping. Additionally, they can use analytics software to analyze data from patient records and identify trends that may suggest an underlying problem or condition.
Nurses should also consider using artificial intelligence (AI) technologies such as natural language processing and machine learning to assist with diagnosis. AI-based systems can help identify patterns in patient data that may lead to a more accurate diagnosis. This can help nurses make better decisions about treatment plans and provide better care to their patients.
As healthcare technology continues to evolve, nurses must stay up to date on the latest trends in nursing diagnosis. By understanding evidence-based practices, developing an evidence-based care plan, and utilizing the latest advanced technologies, nurses can ensure that they are providing quality care to their patients. Additionally, by streamlining processes and making accurate diagnoses, nurses can help improve patient outcomes and create a healthier world.
Conclusion: A Look Ahead to 2023 and Beyond
Nursing diagnosis is an essential component of providing quality care, and it will continue to evolve as healthcare technology advances. In 2023, we can expect nurses to be equipped with the latest tools to streamline processes and help improve patient outcomes. By understanding evidence-based practices, developing detailed assessment plans, and utilizing advanced technologies such as electronic health records (EHRs) and artificial intelligence (AI), nurses can ensure that they are providing the best possible care to their patients.
Looking ahead to the years beyond 2023, nursing diagnosis will continue to be a critical part of providing quality care. With new technologies coming on the market every day, nurses must stay up-to-date with the latest tools and techniques for making accurate diagnoses and developing effective treatment plans.
By continually educating themselves and implementing evidence-based practices, nurses can ensure that they are doing their best to promote positive outcomes for their patients.
In addition, nurses should continue to take advantage of technology by utilizing EHRs and AI systems whenever possible. This will help to streamline processes and reduce errors while also ensuring that the best care is being provided to each patient. Finally, nurses should ensure they are always documenting their work so they can review progress over time and make adjustments based on patient needs. With these practices in place, nurses can improve patient safety and outcomes and create a healthier world.
